The key difference lies in their root causes: osteoarthritis stems from natural joint wear-and-tear, while rheumatoid arthritis is an autoimmune disease where your body attacks its own joints. You’ll notice osteoarthritis typically affects single, weight-bearing joints gradually, whereas rheumatoid arthritis strikes symmetrically on both sides of your body and can progress rapidly. Symptoms also differ: rheumatoid arthritis morning stiffness lasts longer than an hour and may include systemic effects like fever. Recognizing these distinctions guarantees proper treatment and management.
Understanding the Root Causes

Pain is an unfortunate companion for millions of Americans living with arthritis, but understanding the distinct root causes of osteoarthritis and rheumatoid arthritis is essential for proper treatment.
While osteoarthritis results from the natural deterioration of joint cartilage over time, rheumatoid arthritis is an autoimmune disease where your immune system attacks your joints, causing severe joint inflammation. This fundamental difference explains why rheumatoid arthritis can progress rapidly, while osteoarthritis develops gradually.
Your risk factors for rheumatoid arthritis include genetic predisposition, environmental triggers, hormonal changes, and lifestyle choices like smoking and obesity. Given the aggressive nature of this autoimmune disease, early intervention is indispensable to prevent permanent joint damage. Understanding these distinct causes helps you and your healthcare provider determine the most effective treatment approach for your specific condition.
Recognizing Key Symptoms and Warning Signs

Distinguishing between osteoarthritis and rheumatoid arthritis starts with recognizing their unique symptom patterns. These common types of arthritis present distinctly different warning signs that you’ll need to monitor.
- Morning stiffness in RA tends to last over an hour, while osteoarthritis stiffness typically subsides within 30 minutes of waking
- Joint pain in rheumatoid arthritis occurs symmetrically, affecting both sides of your body simultaneously
- Early RA tends to manifest with systemic symptoms like fatigue, low-grade fever, and anemia before joint symptoms appear
- Osteoarthritis typically affects isolated joints, particularly those bearing weight or subjected to repetitive stress
These distinctive patterns help rheumatologists make accurate diagnoses and develop targeted treatment plans. If you’re experiencing persistent joint pain or stiffness, seeking prompt medical evaluation is vital for proper management.
Joint Patterns and Areas of Impact
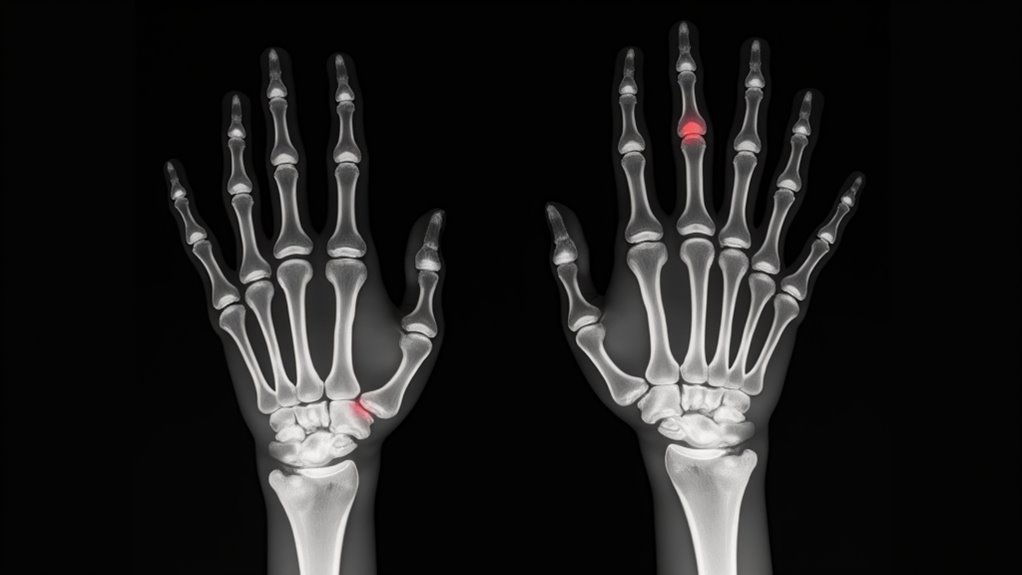
Understanding where arthritis strikes in your body provides essential diagnostic clues. If you’re experiencing joint pain in a single location, particularly in weight-bearing areas like your knees, hips, or spine, you’re likely dealing with osteoarthritis. This condition typically affects one joint at a time and stays localized to that area.
In contrast, rheumatoid arthritis (RA) follows a distinctly different pattern. You’ll notice symmetrical joint involvement, meaning if your right hand is affected, your left hand will likely show similar symptoms. RA commonly targets your hands, wrists, and feet, and it’s not limited to just your joints. Unlike osteoarthritis’s isolated impact, RA can cause widespread inflammation throughout your body, affecting multiple joints simultaneously and potentially impacting other body systems.
Treatment Approaches and Management
You’ll find distinct treatment approaches for osteoarthritis and rheumatoid arthritis, with early intervention being critical for rheumatoid arthritis to prevent permanent joint damage through disease-modifying drugs. While both conditions may require NSAIDs and anti-inflammatories for pain management, rheumatoid arthritis demands more aggressive medication strategies targeting the immune system. Regardless of arthritis type, you should incorporate lifestyle modifications like physical therapy, weight management, and hot/cold therapy to optimize your treatment outcomes.
Early Intervention Strategies
The early intervention strategies for arthritis differ markedly between osteoarthritis and rheumatoid arthritis, although both conditions benefit from prompt medical attention. With rheumatoid arthritis, you’ll need to start disease-modifying anti-rheumatic drugs early to prevent joint damage and slow progression.
Key early intervention steps include:
- Immediate consultation with a rheumatologist for proper diagnosis and initiation of DMARDs if you’re diagnosed with rheumatoid arthritis
- Implementation of targeted physical therapy programs to maintain joint function and mobility in both conditions
- Adoption of lifestyle modifications, including weight loss and appropriate exercise routines, to reduce joint stress
- Participation in extensive patient education programs to understand your condition, treatment options, and self-management strategies
Early intervention is particularly vital for rheumatoid arthritis, as delayed treatment can lead to irreversible joint damage.
Medication Types Compared
Medication strategies for osteoarthritis and rheumatoid arthritis follow distinctly different paths, reflecting their unique disease mechanisms. For osteoarthritis, you’ll typically receive NSAIDs and pain relievers to manage symptoms, along with occasional steroid injections for flare-ups. These treatments focus on pain relief and maintaining joint function.
In contrast, rheumatoid arthritis requires a more complex treatment approach using multiple medication classes. You’ll need disease-modifying anti-rheumatic drugs (DMARDs) to slow disease progression and prevent joint damage. Your doctor may prescribe traditional DMARDs like methotrexate or newer biologic DMARDs that target specific immune system components. While you might still use NSAIDs for symptom relief, ongoing systemic steroid treatments are often necessary to control inflammation. The goal is to achieve remission through this extensive medication strategy.
Lifestyle Management Tips
Effectively managing arthritis requires a thorough lifestyle approach beyond medication alone. According to Health Publishing, you can greatly reduce pain and improve mobility through targeted lifestyle modifications, whether you’re dealing with osteoarthritis or rheumatoid arthritis.
- Engage in regular physical therapy and exercise routines that focus on joint flexibility and strength – these activities help decrease pain and stiffness while maintaining function
- Maintain a healthy weight through proper nutrition, as excess pounds put unnecessary stress on weight-bearing joints
- Work with a physical therapist to develop specific exercises that target your affected joints without causing additional strain
- Incorporate low-impact activities like swimming or cycling that allow you to stay active while minimizing joint pain and protecting vulnerable joints
Risk Factors and Prevention Strategies
Understanding your risk factors is essential for both osteoarthritis and rheumatoid arthritis, with maturity, obesity, and genetics playing key roles in osteoarthritis, while smoking and autoimmune conditions increase your likelihood of developing rheumatoid arthritis. You can substantially reduce your osteoarthritis risk through weight management, regular exercise, and protecting your joints from injury. If you’re concerned about rheumatoid arthritis, you’ll want to focus on avoiding tobacco use and managing any existing autoimmune conditions while working closely with a rheumatologist for early intervention.
Common Risk Factors
Both osteoarthritis and rheumatoid arthritis share several risk factors, though each condition has its distinct triggers and predisposing elements. Understanding these risk factors can help you identify your susceptibility to either condition and take appropriate preventive measures.
Key risk factors that you should be aware of include:
- Physical factors: Obesity and joint injuries primarily increase your risk of osteoarthritis, while aging affects both conditions
- Genetic predisposition: Your family history can influence the development of both types of arthritis, with stronger genetic links to rheumatoid arthritis
- Gender considerations: Women are more likely to develop rheumatoid arthritis than men
- Lifestyle choices: Smoking drastically increases your risk of rheumatoid arthritis, while excessive joint stress from certain activities can lead to osteoarthritis
Prevention Measures That Work
While neither type of arthritis can be completely prevented, you can drastically reduce your risk by implementing targeted prevention strategies based on specific risk factors.
For osteoarthritis prevention, you’ll want to maintain a healthy weight and protect your joints from injuries during physical activities. Regular, low-impact exercise strengthens the muscles around your joints while helping you manage your weight. If you’re overweight, losing excess pounds enormously reduces stress on weight-bearing joints.
For rheumatoid arthritis prevention, focus on addressing modifiable risk factors. If you smoke, quit immediately, as smoking increases your risk tremendously. Don’t ignore your oral health – treating gum disease promptly may lower your rheumatoid arthritis risk. In addition, managing inflammation through a balanced diet and regular physical activity can help reduce your risk of developing both types of arthritis.
Living Well With Arthritis: Daily Tips and Adaptations
Living successfully with arthritis requires an inclusive approach to daily activities and lifestyle alterations. Whether you’re dealing with morning stiffness or diverse types of arthritis, maintaining independence and quality of life depends on implementing effective management strategies.
Managing arthritis effectively means adapting daily routines and lifestyle choices to maintain independence and enhance quality of life.
- Engage in appropriate physical activities: Regular exercise and strength training can improve joint function while reducing arthritis pain
- Apply therapeutic interventions: Utilize heat/cold therapy and topical treatments when needed for symptom relief
- Modify your environment: Use assistive devices and adapt daily tasks to protect your joints from unnecessary strain
- Maintain comprehensive health: Focus on weight management, proper nutrition, and regular consultations with healthcare providers
These evidence-based approaches, combined with support from occupational therapists and arthritis organizations, can help you effectively manage your condition while staying active and independent.
Frequently Asked Questions
How Do I Know if It’s Osteoarthritis or Rheumatoid Arthritis?
You’ll need to ponder several key factors: joint pain severity, joint inflammation levels, and onset of symptoms. Check if your pain affects multiple joints symmetrically (typically rheumatoid) or single joints (usually osteoarthritis). Note how long morning stiffness lasts and whether you experience systemic symptoms like fatigue. Your family medical history and affected joint locations are also meaningful indicators. However, you’ll need a rheumatologist’s evaluation for a definitive diagnosis.
What Type of Arthritis Is the Most Painful?
Based on joint inflammation severity and symptom progression monitoring, rheumatoid arthritis is typically considered the more painful form. You’ll likely experience intense, throbbing pain due to the autoimmune attack on your joints. Pain management techniques are indispensable as the underlying causes examination reveals severe inflammation that can persist for days. Your lifestyle impact assessment may show greater disability compared to other types of arthritis, making early treatment essential for controlling symptoms.
What Are the Four Stages of Osteoarthritis?
You’ll experience four distinct stages of osteoarthritis as joint degeneration progresses. Stage 1 begins with minor cartilage breakdown and small bone spurs. In Stage 2, you’ll notice increased synovial inflammation and further cartilage wear. Stage 3 brings significant functional impairment as cartilage loss becomes severe. Ultimately, Stage 4 represents end-stage disease, where you’ll have extensive cartilage destruction, large bone spurs, and severe joint damage causing significant pain and disability.
What Are 5 Symptoms of Osteoarthritis?
You’ll notice five key symptoms when you have osteoarthritis. The most common is joint pain that typically worsens with activity and improves with rest. You’ll experience joint stiffness, particularly in the morning or after periods of inactivity. You may also notice swelling around affected joints and decreased mobility that limits your range of motion. Supplementary, you might hear or feel crepitus a grinding or crackling sensation when moving the affected joint.





